Implementing Developmental-Behavioral Screens in Primary Care
Probably the most challenging aspect of adopting quality approaches to screening/surveillance is figuring out how to make it work in our practices. There are many considerations but there are also many effective models.
For a downloadable workflow template to aid you in figuring out a viable step-by-step plan–in light of your clinic’s staffing patterns and equipment, please click here. On this page you will also find an example of clinic work-flow chart and information about billing/coding for optimal reimbursement.
How do clinics implement online screening?
The 5 approaches to implementation described below are from a study (Glascoe, 2014) of 79 clinics serving 20, 941 families with a wide-range of backgrounds -from affluent parents to low-income, and from English-speaking to non-English speaking. Although the focus is on use of PEDS Online®, the same processes are applicable when using tools in print, i.e., just add scoring and report writing into the clinic workflow.
- Parent Portal. Parent portals have a number of advantages: Families can complete screens prior to the visit but do not see results. Rather, these are sent directly to clinicians who in turn, have advance notice as to whether referrals are needed, the focus of anticipatory guidance and developmental-promotion. Parent portals enable providers to enter encounters armed with brochures about referral resources, parenting guidance such as specific hand-outs of topics of interest to families, and to practice, if needed, on explaining results.
The PEDS Online® parent portal through which parents can complete screens prior to encounters, was used by 24 of the 79 clinics that collectively screened 2,086 children (10% of the 20,941). Of the 24 clinics, 15 were private practices and 5 were community or public health clinics. Parents accessing the portal were more likely to be English-speaking [OR = 3.2, 95%CI (1.61 - 6.32), p < .0001]. Otherwise there were no differences in presence or absence of portal use due to parents’ level of education or poverty level. Of the 24 clinics, 20 clinics garnered uptake in 56% to 100% of all families, while the remaining 4 clinics had uptake rates of 34% or less.
Approaches to Portal Use
Clinics encouraged families to use the portal in two different ways:
- Having a waiting room computer kiosk or providing parents with tablet computers at check-in so that families could complete screens in the waiting room on the day of the encounter; or
- Giving parents an appointment reminder card including information on how to login to the PEDS Online® website together with a request to complete screens before the next scheduled visit.
Uptake on Portal Use.
Of the two approaches, the clinics with the highest uptake on portal usage were those providing computers in the waiting room (56%, N = 1169 /2086). The 4 clinics with lower rates of portal usage (44%, N = 917/2086) used the appointment reminder approach.
Staffing Patterns and Portal Use. Clinics with computers in waiting rooms, often had waiting room attendants (usually gap year students or retirees paid close to minimum wage) to help parents use computers, probe literacy (by asking if parents preferred assistance), and interview families with limited literacy (e.g., by reading questions aloud). Many of the waiting room attendants were also charged with entertaining children, modeling appropriate adult-child interactions (such as talking to children about their activities), and in many cases implementing Reach and Read, i.e., by reading children’s books aloud so that parents could complete screens undisturbed.
- Interview. Seven clinics administered PEDS Online® exclusively by interview to 16% of all patients in the study sample (N=3,313/20,941). Clinic types included emergency room/crisis call centers, private practices and community/public health centers. Interview administrations were more common when families did not speak English [OR = 1.8, 95%CI (1.01 - 3.22), p < .05] or had elevated poverty levels [OR = 2.0, 95%CI (1.11 - 3.65), p < .02].
Approaches and Staffing Patterns:
- Some clinicians, once entering the exam room preferred to begin with PEDS Online® screens by interview, as an opening to the encounter. In these cases providers gave live interviews while recording responses onto the PEDS Online® website.
- For clinics working with non-English speaking families, the presence of bilingual (most often English-Spanish speaking) staff was common. Bilingual staff was varied in professional backgrounds and included physicians, skilled nurses, med techs, and receptionists.
- In some clinics, families were scheduled for well-visit appointments on days when bilingual staff were present. Group well-visits were reported by one clinic that had limited bilingual staff via a “Spanish (other other) Language Day”.
- When bilingual staff were not available, or when clinics cared for families who spoke neither English nor Spanish, interpretive/translation services were used. Telephone services were the most common method and their personnel were provided written translations of PEDS Online® measures, and then engaged in a three-way call with families and clinic staff, providing back-translation into English. Clinic staff (who were varied in terms of professional backgrounds but most often included skilled nurses) then entered parents’ responses into PEDS Online®.
- Paper-pencil in waiting or exam rooms together with PEDS Online®. This is one of the more commonly used telephone interpretation services. The balance of practices (48/79) whether interviewing only a portion of families or making partial use of the parent portal, administered screens by asking parents to complete printed copies of screens in waiting rooms (74% of all families, N = 15548/20941). After parents completed measures, responses were entered by clinic staff into PEDS Online® to obtain results.
Approaches and Staffing Patterns:
- In some clinics, clipboards were pre-prepared with print-outs of PEDS Online® screens, often together with other surveys (such as a checklist of Bright Futures topics, screens for parental depression/psychosocial risk, the 5-2-1-0 obesity checklist, etc.). Receptionists were often charged with disseminating clipboards/measures at check-in.
- In several large clinics, receptionists were consumed with patient registration and check-out, and so the med tech station served as the point for disseminating clipboards/measures (in many clinics, several families were in the med tech’s room at the same time and thus had at least some time to complete measures while they waited).
- Next, skilled nurses positioned at (much more private) nursing stations entered parents’ responses into PEDS Online®, offering an interview if forms were incomplete or if evidence of limited literacy was present (e.g., no words written on the PEDS Response Form, skipped questions on other measures). Also nurses often clarified parents’ comments and answers to items and pasted final results into EHRs or printed out for paper charts.
- Completion of measures in exam rooms sometimes occurred but more frequently in those clinics where nurses or other staff accompanied families into exam rooms, helped them finish partially completed forms, gathered responses by interview or on paper, entered results into PEDS Online®, and also gathered vital health information. In these cases, computers in the exam room were often available (or were brought in by staff), EHRs in use, and staff often left the EHR age-specific encounter form open along side the PEDS Online® website showing results. In clinics without EHRs, staff entering exam rooms, most often nurses, ensured that paper-pencil forms were complete, and then left the exam room with screening test forms to enter information and print-out results to attach to paper charts.
- Hands-on Screening. Some providers preferred to directly administer PEDS:DM® items to children. Although this was rare, teaching hospital clinics and practices working with medical and nursing students reported using this approach to ensure that trainees mastered skills in behavior management and learned critical milestones. Although not represented in this study, by report, many early intervention intake services, developmental-behavioral and subspecialty clinics also used hands-on administration for training purposes, to gain more detailed insight into children’s challenges, and to meet program/measurement requirements.
- Gated Screening. A few practices used a gated screening process wherein PEDS Online® was used as the front-line series of screens. Children performing poorly were then seen by a nurse practitioner or developmental specialist for additional assessment. Measures included the Brigance Screens (Brigance, 2014). and the PEDS:DM® Assessment Level® (Glascoe & Robertshaw, 2007). A few sites used the Denver-II although this measure has limited accuracy and should be avoided especially when clinics train young professionals and should set an evidence-based example (Glascoe, Byrne, Chang et al, 1992).
Other interesting findings from this study:
Children screened outside the well-visit schedule are at greater risk
Most children, 66% (N = 13,859), were screened at ages coinciding with the AAP’s periodicity schedule (+ 1 month), i.e., at ~ 2 , 4, 6, 9, 12, 15, 18, 24, 36, 48, 60, 72, and 84 months. Nevertheless, 34% (N = 7,082) were screened between well-visit ages, indicating substantial use of opportunistic screening/surveillance. Interestingly, children screened outside the well-visit schedule were 1 ½ times more likely to perform poorly on one or more screening tests [OR = 1.6, 95%CI (1.50 - 1.67), p < .0001].This finding should elevate “the index of suspicion” when children arrive between the usually scheduled visits.
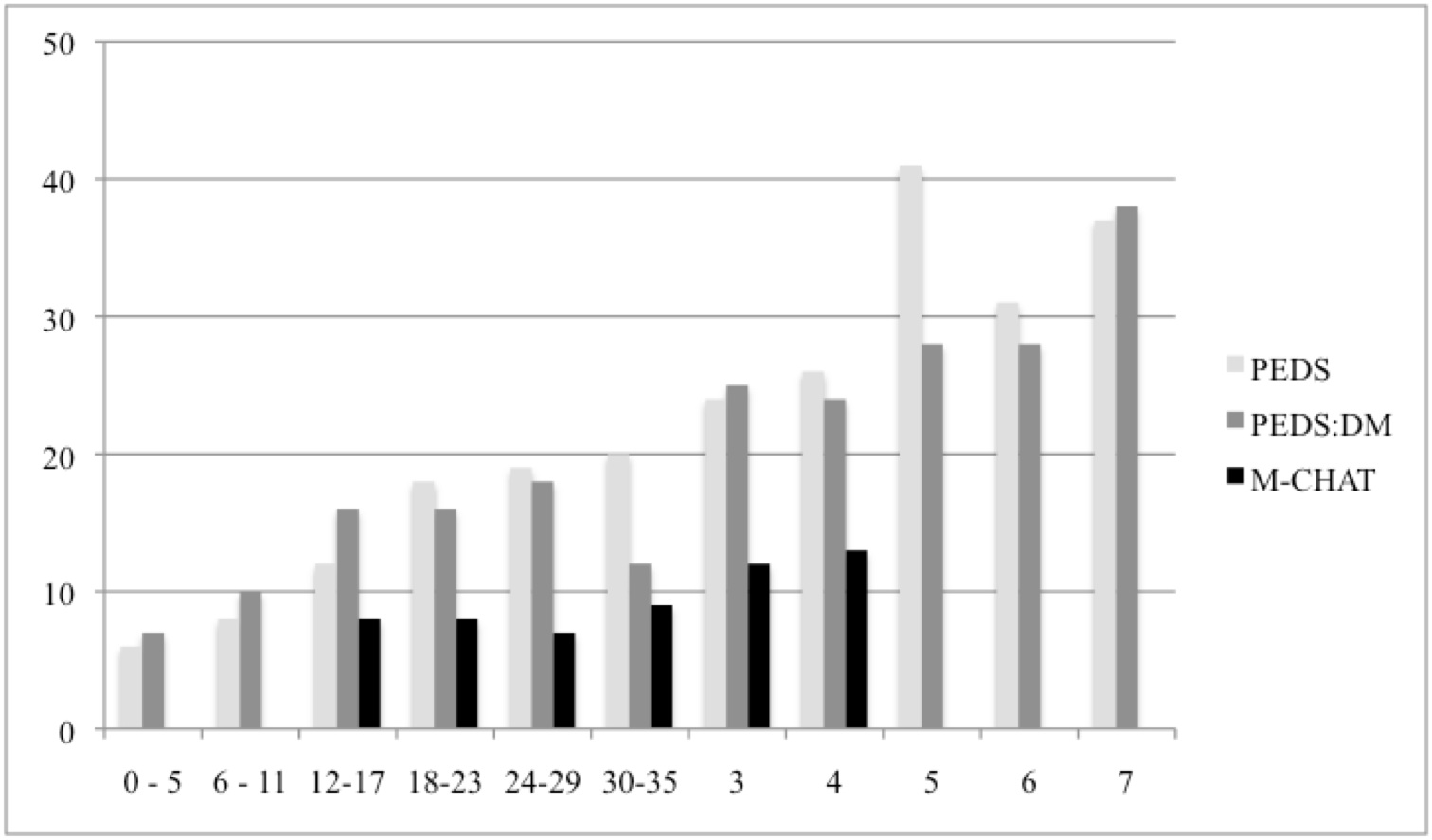
The older the child, the greater the likelihood of failing screens
The figure below shows the percentage of children with high/moderate risk scores on PEDS, two or more milestones unmet on the PEDS:DM®, and failing scores on the M-CHAT. Visible is the known and predictable increase in delays as children’s age increases (Newachek, Strickland, Shonkoff et al, 1998). Children 3 years and older were twice as likely to perform poorly on screens than were children in the birth through 2 year age range [OR = 2.3, 95%CI (2.12 - 2.43), p < .0001]. Thus, we really need to work hard to ensure that children return for well visits, most especially after 2 years of age where attendance drops substantially.
Percentage of Problematic Performance by Age and Screening Test
References
American Academy of Pediatrics Task Force on Mental Health. Enhancing pediatric mental health care: strategies for preparing a primary care practice. (2010). Pediatrics, 125(suppl 3): S87-S108.
American Academy of Pediatrics. (2006). Identifying Infants and Young Children With Developmental Disorders in the Medical Home: An Algorithm for Developmental Surveillance and Screening. Pediatrics, 118(1):405-20.
American Academy of Pediatrics. (2009). The Future of Pediatrics: Mental Health Competencies for Pediatric Primary Care. Pediatrics, 124(1):410-21.
Anderson, L.M., Shinn, C., Fullilove, M.T., Scrimshaw, S.C., Fielding, J.E., Normand, J. (2003). The effectiveness of early childhood development programs: A systematic review. American Journal of Preventive Medicine, 24(3):32-46.
Baio, J. (2008). Prevalence of Autism Spectrum Disorders: Autism and Developmental Disabilities Monitoring Network, 14 Sites, United States, 2008. Centers for Disease Control and Prevention: Morbidity and Mortality Weekly Report. Surveillance Summaries, 61(3): 1-19.
Baron, R.J. (2010). What’s keeping us so busy in primary care? A snapshot from one practice. New England Journal of Medicine, 362:1632-1636.
Bethell, C., Reuland, C., Schor, E., Abrahms, M., Halfon, N. (2011). Rates of parent-centered developmental screening: disparities and links to services access. Pediatrics, 128(1):146-55.
Brothers, K., Glascoe, F.P., Robertshaw, N.S. (2008). Validation of a developmental milestones checklist for primary care. Clinical Pediatrics, 47; 271-279.
Boyle, C.A., Boulet, S., Schieve, L.A., Cohen, R.A., Blumberg, S.J., Yeargin-Allsopp, M. (2011). Trends in the Prevalence of Developmental Disabilities in US Children, 1997-2008. Pediatrics, 127(6):1034-42.
Brigance, A. (2014). Brigance Screens-III. North Billerica, MA: Curriculum Associates.
Campbell, F.A., Ramey, C.T., Pungello, E., Sparling, J., Miller-Johnson, S. (2002). Early childhood education: Young adult outcomes from the Abecedarian Project. Applied Developmental Science, 6(1):42-57.
Cox, J.E., Huntington, N., Saada, A., Epee-Bounya, A., Schonwald, A.D. (2010). Developmental Screening and Parents’ Written Comments: An Added Dimension to the Parents’ Evaluation of Developmental Status Questionnaire. Pediatrics, 126 (Supplement 3): S170-S176.
Farran, D.C. (2005). Developing and implementing preventive intervention programs for children at risk: Poverty as a case in point. In M. Guralnik (ED.) The developmental systems approach to early intervention. (pp 267 - 304). Baltimore, MD: Brookes Publishing Co.
Glascoe, FP. (2014). Evidence-Based Early Detection of Developmental-Behavioral Problems in Primary Care: What to Expect and How to Do It. Journal of Pediatric Child Health. in press.
Glascoe, F.P., Byrne, K.E., Chang, B., Strickland, B., Ashford, L., Johnson, K. (1992). The Accuracy of the Denver‑II in Developmental Screening. Pediatrics, 89:1221‑1225.
Glascoe, F.P., Dehnert, M., Poon, J.K. (2014). Economics of Developmental-behavioral Services in Primary Care. Pediatrics. 2014, submitted.
Glascoe, F.P., Marks, K.P., Poon, J.K., Macias, M.M. (2013) (eds), Identifying and Addressing Developmental-Behavioral Problems: A Practical Guide for Medical and Non-medical Professionals, Trainees, Researchers and Advocates. Nolensville, Tennessee: PEDStest.com, LLC, www.pedstest.com.
Glascoe, F.P., Robertshaw, N.S. (2007). Parents’ Evaluation of Developmental Status: Developmental Milestones (PEDS-DM). Nolensville, Tennessee: PEDSTest.com, LLC.
Glascoe, F.P. (2013). Collaborating with Parents: Using Parents’ Evaluation of Developmental Status in Early Detection and Intervention. (2nd edition). Nolensville, Tennessee: PEDSTest.com, LLC.
Glascoe, F.P. (2012). Parents’ Evaluation of Developmental Status (PEDS). Nolensville, Tennessee: PEDSTest.com, LLC.
Guevara, J.P., Gerdes, M., Localio, R., Huang, Y.V., Pinto-Martin, J., Minkovitz, C.S. (2013). Effectiveness of Developmental Screening in an Urban Setting. Pediatrics, 131(1):30-7.
Halfon, N., Stevens, G.D., Larson, K., Olson, L. (2011). Duration of a Well-Child Visit: Association With Content, Family-Centeredness, and Satisfaction, Pediatrics, 128:657-664.
High, P.C., the Committee on Early Childhood, the Committee on Early Childhood, Adoption, and Dependent Care and Council on School Health. School Readiness. (2008). Pediatrics, 121(4):e1008-e15.
Hix-Small, H., Marks, K., Squires, J., Nickel, R. (2007). Impact of Implementing Developmental Screening at 12 and 24 Months in a Pediatric Practice. Pediatrics, 120(2):381-9.
Muennig, P., Schweinhart, L., Montie, J., Neidell, M. (2009). Effects of a prekindergarten education intervention on adult health: 37-year follow-up results of a randomized controlled trial. American Journal of Public Health, 99(8), 1431-1437.
Myers, S.M., Johnson, C.P., the Council on Children with Disabilities. Management of Children With Autism Spectrum Disorders (2007). Pediatrics, 120(5):1162-82.
NAPNAP Position Statement on Pediatric Health Care/Medical Home: Key Issues on Delivery, Reimbursement, and Leadership. (2009). Journal of Pediatric Health Care, 23: 23A - 24A.
NAPNAP Position Statement on the Integration of Mental Health Care in Pediatric Primary Care Settings. (2013a). Journal of Pediatric Health Care, 27:15a-16a.
NAPNAP Position Statement on the PNPs Role in Supporting Infant and Family Well-Being During the First Year of Life. (2011). Journal of Pediatric Health Care, 25: 9A - 11A.
NAPNAP Position Statement on the Role of Pediatric Nurse Practitioners in Quality Improvement (2013b). Journal of Pediatric Health Care, 27: e43 - e45.
Newachek, P.W., Strickland, B., Shonkoff, J.P., Perrin, J.M., McPherson, M., McManus, M., Lauver, C., Fox, H., Arango, P. (1998). An epidemiological profile of children with special health care needs. Pediatrics, 102:117-23.
Noritz, G.H., Murphy, N.A., Neuromotor Screening Expert Panel. Motor Delays: Early Identification and Evaluation. (2013). Pediatrics, 131:6 e2016-e2027
Radecki, L., Sand-Loud, N., O’Connor, K.G., Sharp, S., Olson, L.M. (2011). Trends in the use of standardized tools for developmental screening in early childhood: 2002-2009. Pediatrics, 128(1):14-9.
Reynolds, A.J., Temple, J.A., Ou, S.R., Arteaga, I., White, B. (2011). School-Based Early Childhood Education and Age-28 Well-Being: Effects by Timing, Dosage, and Subgroups. Science, 333(6040):360-364.
Reynolds, A.J., Temple, J.A., White, B., Ou, S., Robertson, D.I. (2011). Age-26 cost-benefit analysis of the Child-Parent Center early education program. Child Development, 82(1):379-404.
Robins, D., Fein, D., Barton, M. (1999). The Modified Checklist of Autism in Toddlers. Storrs, CT: University of Connecticut. www.mchatscreen.com.
Schonwald, A., Horan, K., Huntington, N. (2009). Developmental Screening: Is There Enough Time? Clinical Pediatrics, 48(6):648-55.
Schonwald, A., Huntington, N., Chan, E., Risko, W., Bridgemohan, C. (2009). Routine Developmental Screening Implemented in Urban Primary Care Settings: More Evidence of Feasibility and Effectiveness. Pediatrics, 123(2):660-8.
Schweinhart, L.J., Montie, J., Xiang, Z., Barnett, W.S., Belfield, C.R., Nores, M. (2005). Lifetime effects: The HighScope Perry Preschool study through age 40. Monographs of the HighScope Educational Research Foundation. Ypsilanti, MI: HighScope Press.
Selden, T.M. (2006). Compliance With Well-Child Visit Recommendations: Evidence From the Medical Expenditure Panel Survey, 2000-2002. Pediatrics, 118: e1766-e1778.
Sices, L., Feudtner, C., McLaughlin, J., Drotar, D., Williams, M. (2003). How do primary care physicians identify young children with developmental delays? A national survey. Journal of Developmental Behavioral Pediatrics, 24(6):409-17.
Simon, A.E., Pastor, P.N., Avila, R.M., Blumberg, S.J. (2013). Socioeconomic disadvantage and developmental delay among US children aged 18 months to 5 years. Journal of Epidemiology and Community Health, 67(8):689-95.
Stevens, G.D. (2006). Gradients in the health status and developmental risks of young children: the combined influences of multiple social risk factors. Maternal and Child Health Journal, 10:187-99.
